By David L. Johnson, NHA, RAC-CT
As a senior quality improvement specialist with IPRO, the Quality Improvement Organization for New York State over the past 11 years, I’ve been tasked with helping skilled nursing facilities (SNFs) embrace the process of continuous quality improvement. A necessary component of this effort has been to collect, understand, and analyze timely and accurate data. This article discusses a free tool I developed to help SNFs track their data related to pressure ulcers and focus their quality improvement efforts for the greatest impact.
The beginning
Since 2002, the quality initiatives administered by CMS have included the prevention and treatment of pressure ulcers as a focus topic for SNFs across the country. The challenge has been to guide identified facilities to collect their own data, in real time, and drill down into that data to identify trends and opportunities for improvement.
In 2002, I decided to develop a tracking tool to help SNFs with the timely collection of their pressure ulcer data. The tool had to be in a format that could be easily used by most providers, including those with basic computer equipment and operating skills. The purpose of this tracking tool was not to replace the necessary clinical documentation of the pressure ulcers, but to offer a focused document with pertinent statistical information for all cases of pressure ulcers in the SNFs at any point in time.
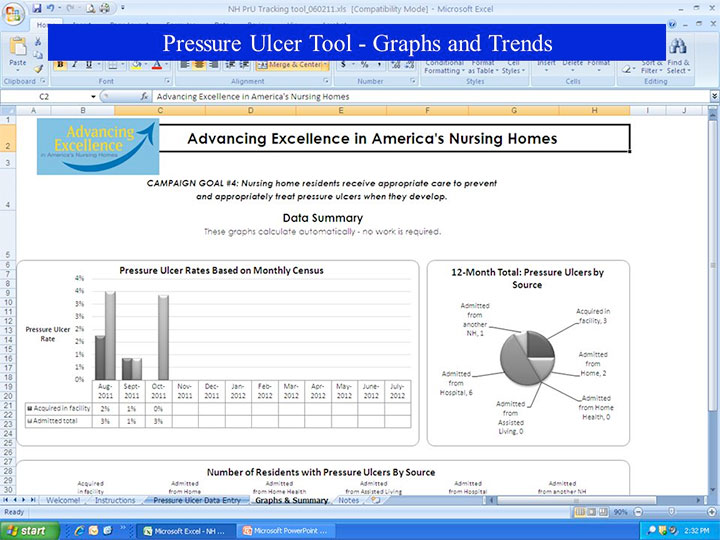
The current Monthly Pressure Ulcer Tracking Form is in its fifth generation. First developed in an Excel 2003 format, the original tracking tool was very functional, but basic. However, Excel 2007 enabled me to add functionality that launched the originally developed tool into a format offering not only a detailed summary and graphs for the entire SNF but also instant access to individual summaries and related graphs for up to 15 separate user-defined locations. For example, those designated locations could be as general as individual units or as detailed as specific care assignments.
How it works
The current version of the Monthly Pressure Ulcer Tracking Form offers the convenience of an Excel spreadsheet to instantly summarize and graph your pressure ulcer data by such categories as site, origin, stage, age of wound (auto-calculated), days to heal (auto-calculated), and weekly response to treatment. The tracking form also summarizes all wounds that are new for the month, by both site and stage and by whether they developed in-house or were present on admission. (See Sample data calculation and graph for all acquired in-house pressure ulcers by stage.)
All of the printed summaries and graphs are clearly identified by their user-defined facility location. Users can quickly identify the data source with the opportunity to easily detect both adverse trends and their own program successes.
Built-in macros for the tracking form walk the user through everything from adding a new case to an end-of-month routine that conveniently saves the data in the current monthly file. The macros then remove the information for all healed or discharged pressure ulcer cases before carrying over all of the data on existing pressure ulcers for the start of a new month of tracking.
All wounds are entered only once, and the weekly status update is as simple as a single letter code for “new,” “improved,” “same,” “worsened,” or “healed.” The data format was intentionally built to allow these factual entries to be clerically entered after collection and assessment by the appropriate professional.
The user is guided through the data entry process with helpful hints in cell drop-down menus as well as embedded data validation rules to restrict what is entered, thereby offering a summary and analysis true to the expectations and spirit of the tracking form.
Efficient data collection in real time is invaluable to wound care teams, offering them the potential to immediately identify adverse trends or celebrate small successes in their wound care program. Take, for example, a calculated increase in facility-acquired stage 2 pressure ulcers. Is there a common site? Is the increase isolated to one designated location or unit? Are there opportunities for focused education efforts, such as early identification or proper prevention practices? The ability to drill down into your data will allow you to focus your limited resources in the areas of identified documented need. (See Sample data calculation and graph for all healed pressure ulcers by site.)
In another example, the data analysis offered instantaneously through this tracking form can easily compare data among designated units within your facility. Is there a unit experiencing better healing times? Has there been a unit experiencing no facility-acquired pressure ulcers? What does that tell you about its prevention practices? How can those practices be spread?
A free resource
In summary, the timely collection, analysis, and attention to your facility’s pressure ulcer data can be invaluable in your internal quality improvement efforts.
These tracking forms are available for download free of charge at nursing
homes.ipro.org under “Clinical Topics, Pressure Ulcer Clinical Tools and Resources.” You can download a tracking tool with sample data (for demonstration and training purposes), a master blank file for immediate facility implementation, and a multipage PDF desk-side instructional booklet. The instructional booklet offers simple, clear instruction with actual screen prints to help guide the user through the tracking tool functionality. The original tracking tool written in Excel 2003 is still available for those providers with Excel versions earlier than 2007. However, the functionality of the latest generation, which is available to anyone with Excel 2007 or newer, is far superior and highly recommended.
For additional information, please e-mail me at [email protected].
Note: This material was prepared by IPRO, the Medicare Quality Improvement Organization for New York State, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents do not necessarily reflect CMS policy. 10SOW-NY-AIM7.2-14-24.
David L. Johnson is a senior quality improvement specialist with IPRO, the Quality Innovation Network-Quality Improvement Organization for New York State.
Disclaimer: The views expressed in this article are those of the author and do not necessarily represent the views of, and should not be attributed to, Wound Care Advisor. All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.